By LISA LIDDANE
The Orange County Register
Sunday, September 19, 2004

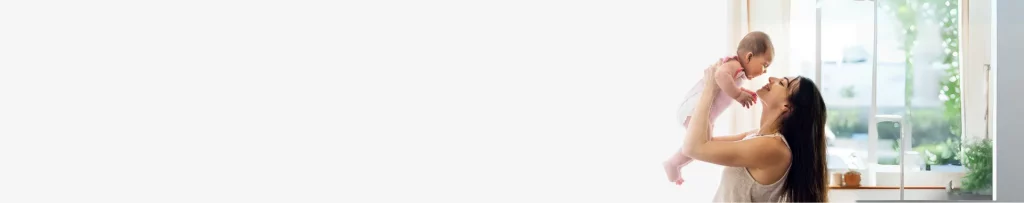
DUE IN DECEMBER: Beatriz Sandoval is eagerly awaiting the birth of her child. “I have calmness throughout this pregnancy,” she says.
SANG H. PARK, THE ORANGE COUNTY REGISTER
For as long as she can remember, Beatriz Sandoval always longed to have children. And as long she could help it, she would not let breast cancer stand in the way.
Sandoval was 32 when she was diagnosed with fast-growing stage 1 breast cancer in 1999. She confronted not just the question of survival but also the question that others like her who are 40 years and younger face: Can I still have a child?
Chemotherapy, a staple of cancer treatment, can cause infertility.
“When my doctor mentioned the risks of chemotherapy damage to the ovaries, the words went beyond my ears and down to the depths of my soul,” she said. “The idea that I might not be able to have a child was much more overwhelming and had a huge impact on my diagnosis.”
There are fertility treatment options, but these have to be weighed carefully against survival issues.
More doctors are discussing these fertility options with patients, but there’s still a long way to go, said Dr. Lynn Westphal, assistant professor at the department of obstetrics and gynecology at Stanford University in Palo Alto. “A lot of women may not get information from their oncologists,” she said. Doctors may be so focused on their patients’ survival that they don’t always bring up fertility options.
Sandoval broached the subject of fertility with her doctor, Dr. Tariq Mahmood at St. Joseph Hospital in Orange.
“When the (doctor) gave my husband and I the diagnosis, he asked if we had any questions. I told him I had only one question: ‘How is this going to affect my ability to nurse a child?’
“He looked surprised and puzzled. Most of the questions he gets when he gives patients the bad news are related to dying. He hesitated only for a second before he deadpanned, ‘Well, it will affect your ability to switch breasts, because you’ll only have one to use.’ “
After Mahmood realized how important childbearing was to Sandoval, they discussed a plan of action. Sandoval turned to Dr. Lawrence Werlin, a reproductive endocrinologist in Irvine. “He understood the urgency of the situation and suggested freezing embryos,” Sandoval said. This was the first part of in-vitro fertilization.
Mahmood identified a small window of opportunity after mastectomy and before chemotherapy and radiation for Sandoval to undergo hormonal treatments to stimulate her ovaries. During that window, Werlin retrieved 16 eggs from Sandoval’s ovaries and fertilized them with sperm from her husband, Jorge Sandoval. Two days later, the couple had 11 viable embryos, which were frozen.
Sandoval began chemotherapy, then segued immediately into radiation. In June 2000, she began taking the drug tamoxifen for 18 months as a cancer preventive measure. The typical tamoxifen regimen lasts five years, but sometimes, oncologists shorten the duration if a couple is considering having children and the patient’s health permits.
In 2002, two years after Sandoval completed her cancer treatment, she and her husband began trying to conceive naturally, but to no avail.
Earlier this year, they decided to continue with the last part of in-vitro fertilization: embryo transfer. While being monitored for any sign of recurrence, Sandoval received hormones to thicken the lining of her uterus, which was needed to support a pregnancy. Werlin implanted four of the Sandovals’ embryos.
Two weeks later, Sandoval learned she was pregnant. Her baby is due just before Christmas.
Surviving breast cancer and coping with fertility challenges, she said, has given her serenity, strength and a sense of what matters.
“I have calmness throughout this pregnancy,” she said. “I understand what’s important. We have a crib in our bedroom. It’s great if you have a nursery you can decorate, but if you can’t have one, that’s OK.
“What’s really important is bringing life into this world. I live for the special moments. I absolutely cherish watching and waiting for my waistline to expand.”
She and Jorge have decided not to find out the sex of their baby.
“Everything we had to do to have this baby was so deliberate, so methodical and clinical that I wanted the chance to experience something traditional, something magical. So I proposed to my husband that we wait until the birth. At first, he asked how we would know what to shop for. I told him that was the least of my worries.
“I have had a lot of time to think about what kind of mother I want to be,” she said. “The last five years have been so full of many trials of different types. I’ve defined my own convictions and have a stronger sense of confidence.
“My greatest hope is that I will able to do everything possible for my child to make sure he or she has a chance to become a remarkable and responsible human being. The rest of it will come in time.”
Julianna Nikolic
Chief Strategy Officer
Julianna Nikolic leads strategic initiatives, focusing on growth, innovation, and patient-centered solutions in the reproductive sciences sector. With 26+ years of management experience and a strong entrepreneurial background, she brings deep expertise to advancing reproductive healthcare.